Headache Treatment

What is a Headache?
A headache is a pain or discomfort in the head, scalp, or neck. It can range from mild to severe and may occur on one or both sides of the head. Headaches can be caused by various factors, including tension, stress, sinus issues, or underlying medical conditions. If not treated, it can greatly reduce the quality of life. Understanding the type and cause of a headache is important for effective treatment. From simple lifestyle changes to medical interventions, there are many ways to manage and ease headache symptoms. Whether occasional or chronic, looking for proper care can help prevent headaches.
Common Causes of Headaches
Headaches can stem from various factors, including:
- Stress and Tension. Emotional or physical stress leading to tension-type headaches.
- Migraine Triggers. Foods, hormonal changes, or sensory stimuli causing migraines.
- Dehydration. Lack of hydration often results in headaches.
- Poor Posture. Strain from improper posture affecting the neck and head.
- Sinus Issues. Inflammation or infection causing pressure and pain.
- Eye Strain. Extended screen time or uncorrected vision problems.
- Sleep Problems. Irregular sleep patterns or poor quality sleep.
- Medical Conditions. Chronic illnesses like high blood pressure or nerve disorders.
Effective headache treatment targets both symptoms and underlying causes for lasting relief.

What is a Facet Joint Injection?
There are various types of headaches that people experience, each with its own causes, symptoms, and treatments. Some headaches are triggered by stress or tension, while others may arise from underlying health conditions or lifestyle factors. Understanding the type of headache you’re dealing with can be helpful in finding the right treatment and managing symptoms effectively.
Cluster Headache Treatment Options
Cluster headaches occur in cycles and are more common in men. They usually begin between the ages of 20 and 40. These attacks can last from 15 minutes to several hours and may occur multiple times a day. Headache treatments for cluster headaches focus on managing pain quickly and preventing future attacks. Options include oxygen therapy, where breathing pure oxygen can help relieve symptoms, as well as medications like triptans or corticosteroids. In some cases, cluster headache specialists may prescribe preventive medications to reduce the frequency.
Sinus Headache Treatment Details
Sinus headaches occur when the sinus cavities in your face become inflamed or congested, usually because of allergies or an infection. This causes pain and pressure around the forehead, cheeks, and eyes. Headache relief for sinus headaches focuses on reducing the congestion and inflammation. Treatments often include decongestants, saline nasal sprays, or antihistamines to ease pressure. Warm compresses applied to the sinus area can also help ease pain. In cases of bacterial infection, antibiotics may be necessary.
Tension Headache Treatment Possibilities
Tension-type headaches are the most common type of headache. Experts estimate that up to 78% of people have experienced them. This type is often caused by stress, muscle tension, or poor posture. They create a dull, aching pain around the forehead or the back of the head and neck. Common ways to relieve headaches like these include over-the-counter pain relievers, such as ibuprofen or acetaminophen. Staying hydrated and taking breaks from screens or stressful activities can prevent these headaches from occurring frequently.
Details on Cervicogenic Headache Treatment
Cervicogenic headaches are caused by issues in the neck, like muscle strain, joint problems, or nerve irritation. The pain often starts at the base of the skull and can spread to the forehead or behind the eyes. Treatment typically includes addressing the neck issue itself. A doctor may recommend physical therapy for cervicogenic headache to improve neck strength and flexibility, manual therapies like chiropractic adjustments, or medications for pain relief. In some cases, nerve blocks or injections may be used.
Post Traumatic Headache Treatment Details
Post-traumatic headaches often occur after a head injury, like a concussion. These headaches can feel similar to tension or migraine headaches, causing dull or throbbing pain. Treatment focuses on finding the best headache relief for each person’s symptoms. Over-the-counter pain relievers are often used first, but if headaches go on, a doctor may prescribe medications similar to those used for migraines. Rest, hydration, and avoiding triggers like bright lights or loud noises can also help. In some cases, physical therapy or relaxation techniques are recommended.
Understanding Thunderclap Headache Treatment
A thunderclap headache is a sudden, severe headache that peaks in intensity within seconds, often described as the “worst headache of one’s life”. It can be a sign of a serious medical issue, like a brain bleed or aneurysm, so it requires immediate medical attention. A headache doctor will usually order imaging tests, like a CT scan or MRI, to find the cause. Treatment depends on the underlying issue but may include medications to control pain and stabilize blood pressure or even surgery if needed. Quick diagnosis and treatment are very important for thunderclap headaches because of their potential seriousness.
Hemiplegic Migraine Treatment
A hemiplegic migraine is a rare type of migraine that can cause temporary paralysis or weakness on one side of the body, along with typical migraine symptoms like severe headache, nausea, or sensitivity to light. It often runs in families, making it a genetically influenced condition. Treatment usually includes medications to prevent or reduce the frequency and severity of attacks, such as calcium channel blockers, anticonvulsants, or tricyclic antidepressants.
Concussion Headache Treatment and How Does it Work
Concussion headaches are common after a head injury and can feel like dull, throbbing pain or intense pressure. These headaches occur as a result of the brain’s reaction to the trauma and may last for days or even weeks. Treatment focuses on managing symptoms and giving the brain time to heal itself. Rest is important, so limiting physical and mental activity helps. Over-the-counter pain relievers may be recommended for temporary relief, but it’s best to avoid heavy medication. Staying hydrated and avoiding bright lights and loud sounds can also help.
What are Pediatric and Adolescent Headache and How to Treat Them
Pediatric and adolescent headaches can range from mild migraines to tension or cluster headaches, and they may sometimes indicate certain health issues. These headaches can cause pain in the forehead, temples, or back of the head and may be accompanied by nausea, fatigue, or sensitivity to light. Treatment usually includes lifestyle changes, such as better sleep habits, hydration, and stress management. Over-the-counter pain relievers like ibuprofen or acetaminophen may help reduce symptoms. For more severe cases, a doctor might recommend prescription medications or therapy.
Rebound Headache Treatment Options
Rebound headaches (also called medication-overuse headaches) happen when pain medications are used too often, causing the headache to return once the medicine wears off. These headaches create a cycle of pain and medication that’s hard to break. Treatment involves gradually reducing or stopping the overuse of medication, better with guidance from a doctor. During this process, other treatments like hydration, rest, and alternative pain relief methods can help. Some people may need a temporary prescription for a different medication to ease withdrawal. Breaking the vicious cycle of rebound headaches can lead to long-term headache relief.
How Does Chronic Headache Treatment Work
Chronic headaches are headaches that occur 15 or more days a month, lasting for months at a time. These can include migraines, tension headaches, or a mix of both. Treating chronic headaches focuses on reducing both frequency and severity. Doctors may prescribe preventive medications, such as antidepressants, anticonvulsants, or beta-blockers. Lifestyle changes, like managing stress, getting regular sleep, and staying hydrated, are also important. Some people benefit from physical therapy, relaxation, or dietary adjustments.
Treating Post-Covid 19 Headache
Post-Covid 19 headaches are lingering headaches experienced after recovering from Covid-19. These headaches can range from mild to severe and are often associated with fatigue, brain fog, or stress. Treatment typically includes over-the-counter pain relievers like ibuprofen or acetaminophen to manage pain. Staying hydrated, maintaining a regular sleep schedule, and reducing stress through relaxation and other means can also help.
Aura Migraine Treatment
A migraine with aura is a severe headache that includes sensory disturbances like visual changes, tingling sensations, or speech difficulties, which occur 10 to 60 minutes before the headache begins. These migraines can cause intense throbbing pain, nausea, and sensitivity to light or sound. Treatment usually includes medications like triptans or nonsteroidal anti-inflammatory drugs (NSAIDs) to ease pain and symptoms during an attack. For preventive measures, options such as beta-blockers, anticonvulsants, or magnesium supplements may be recommended.
What is a New Daily Persistent Headache and How to Treat it
A new daily persistent headache (NDPH) begins suddenly in someone with no prior headache history and involves daily, continuous pain that doesn’t ease. It often feels like a tension headache or mild migraine, with varying intensity. Medications like pain relievers, antidepressants, or muscle relaxants are commonly used. For more severe cases, nerve blocks or cognitive behavioral therapy (CBT) may help.
Understanding Paroxysmal Hemicrania (PH)
Paroxysmal Hemicrania (PH) is a rare headache condition causing short, severe attacks of pain on one side of the head. These headaches can occur chronically (daily) or episodically, lasting from a few minutes to an hour. The pain is often sharp and focused around the eye or temple, sometimes accompanied by tearing or nasal congestion. Treatment usually includes indomethacin, a nonsteroidal anti-inflammatory drug (NSAID) that is highly effective against PH symptoms.
How to Achieve Allergy Headache Relief
Allergy headaches are caused by sinus congestion and inflammation because of allergies, leading to pain and pressure around the forehead, cheeks, and eyes. For allergy headache relief, treatments usually focus on treating allergy symptoms and easing sinus pressure. Antihistamines can help by blocking the body’s allergic response, while decongestants reduce sinus swelling. Nasal sprays or saline rinses can also clear out allergens and reduce congestion. Over-the-counter pain relievers may help with headache pain. Avoiding known allergens, using air purifiers, and staying indoors on high-pollen days can also help.
Menstrual Headache Treatment
Menstrual headaches are linked to hormonal changes during the menstrual cycle and can occur at any point in the cycle. These headaches often feel similar to migraines, with throbbing pain, sensitivity to light or sound, and nausea. Treatment is rather typical and includes pain relievers, like ibuprofen or acetaminophen, to manage symptoms during an episode. If pain is too severe or frequent, preventive treatments such as triptans, hormonal therapies, or magnesium supplements may be recommended.
Pregnancy Headache Relief Details
Pregnancy headaches are common, especially in the first trimester, because of hormonal changes, increased blood flow, and stress. These headaches usually feel like tension headaches with a dull, steady ache. For pregnancy headache relief, doctors recommend safe, non-medicated methods first. Rest, hydration, and gentle exercises can help ease the pain. A cold or warm compress applied to the forehead or neck can also help. Avoiding known triggers, like caffeine or certain foods, also helps. If the headache persists, consult a doctor before taking any medication.

Treatment Options for Headaches
Headaches can vary widely in type and severity, so finding just the right treatment often depends on understanding what’s causing the pain. Treatment options range from lifestyle changes to medications and physical therapies, each to address specific headache triggers and symptoms. A specialist for headaches can help identify the cause and recommend the most effective treatment plan, so you get the relief that best suits your needs.
Medications for Headaches
Medications for headaches are the most simple and common option. It can provide quick and effective relief, especially for common types like tension headaches and migraines. Over-the-counter options, such as ibuprofen, acetaminophen, or aspirin, help ease pain and are often the first choice. For more severe headaches, prescription medications like triptans or beta-blockers may be recommended. Preventive medications, taken daily, can help reduce the frequency of chronic headaches. It’s important to use these medications as directed, as overuse can lead to rebound headaches.
Botox Injections for Migraine
Headache Botox injections are a treatment option for people who suffer from chronic migraines (15 or more days a month). During Botox injections, small doses of Botox are injected into specific areas of the head and neck. This works by blocking pain signals and relaxing muscles, which can reduce the frequency and severity of migraines. Many people find relief after a few sessions, with effects lasting for around three months. Botox injections are especially useful for those who haven’t responded well to other treatments.
Physical Therapy and Lifestyle Adjustments
Physical therapy for headaches focuses on easing muscle tension, improving posture, and flexibility, which can reduce the frequency and intensity of certain types of headaches. Lifestyle adjustments, like getting regular sleep, staying hydrated, and managing stress, also play a big role in headache prevention and treatment. Avoiding common triggers, such as certain foods or long screen time, can further help. Together, physical therapy and lifestyle changes provide a natural, proactive way of managing and preventing headaches.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a type of talk therapy that helps people manage and reduce headaches by changing how they respond to stress and negative thought patterns. During CBT sessions, a therapist guides you in identifying triggers, developing coping strategies, and learning relaxation techniques. By addressing known factors such as strong emotions and stress, CBT can help reduce the frequency and intensity of headaches. It’s especially useful for tension headaches and migraines.
Nerve Block Injections
Nerve block injections are a treatment that helps ease headache pain by blocking specific nerves that send pain signals to the brain. During the procedure, a doctor injects a local anesthetic, sometimes with a steroid, near the targeted nerve. This temporarily “turns off” the pain signals. The effects can last from days to months, depending on the individual. Nerve blocks are a minimally invasive option and are often used for people who haven’t found relief with other treatments.
Benefits of Headache Treatments
Benefits of headache treatments include:
- Pain Relief. Headache treatments offer effective pain relief, helping people get back to their daily activities.
- Reduced Frequency and Severity. Many treatments, such as medications or preventive therapies, aim to reduce how often headaches occur and how bad they feel.
- Natural Options Available. For those looking for a medication-free treatment, options like massage therapy for headaches or physical therapy can help.
- Better Quality of Life. With fewer headaches, people often find they sleep better, feel more energized, and experience less stress.
- Available Customization. Headache treatments are personalized to fit each person’s needs, from lifestyle adjustments to nerve blocks, so the right approach is chosen for each type of headache.
- Addressing Causes. Some treatments work by addressing the causes of headaches rather than just symptoms, like stress or muscle tension, providing better relief.

Potential Risks of Headache Treatments
- Medication Overuse. Taking headache medications too frequently can lead to rebound headaches.
- Side Effects from Injections. Treatments like nerve blocks or Botox injections may cause temporary swelling, soreness, or bruising at the injection site. Though rare, infections or nerve irritation can also happen.
- Temporary Discomfort with Physical Therapy. Physical therapy and other hands-on treatments can sometimes lead to short-term soreness as muscles adjust.
- Overuse of Alternative Therapies. While options like red light therapy for headache can be helpful, overuse or improper use may lead to mild side effects like skin sensitivity or headaches from excessive light exposure.
- Risk of Dependency. Some people may rely too heavily on pain relief options, which can create dependency and make it harder to manage headaches naturally.
- Allergic Reactions. Some individuals may experience allergic reactions to certain medications or injection components.
for your pain needs
Choose Us for Headache Treatment in Chicago, IL
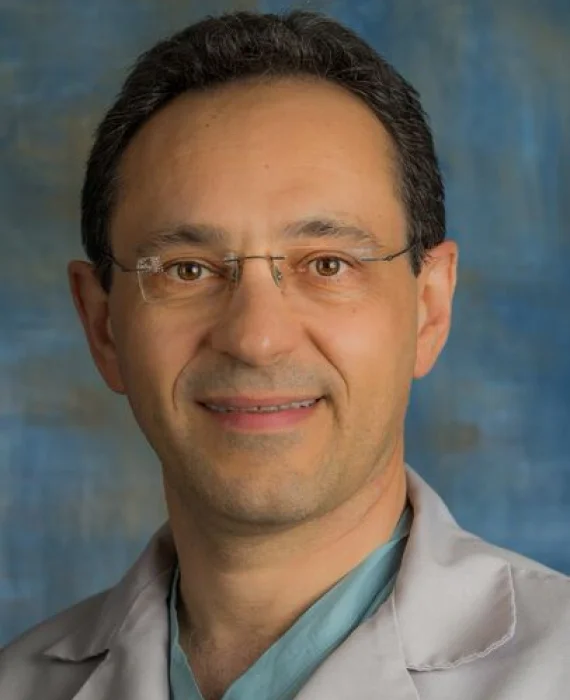
Choose Painless Medical Practice in Chicago, IL, for effective and fully personalized headache treatment. Led by Dr. Jaroslav Tymouch, MD and Founder, our pain management clinic is dedicated to helping you find real relief. As a headache specialist in Chicago, Dr. Tymouch understands that each headache is unique, whether it’s a tension headache, migraine, or cluster headache. He personalizes each treatment accordingly, so it fits your specific needs. The treatment may include a wide range of options, such as medications, injections, physical therapy, and alternative therapies like massage.
With Dr. Tymouch’s expertise as a headache specialist, you’ll receive compassionate, genuine care designed to address the causes of your pain, not just the symptoms. Our goal is to get you back to enjoying life. Ready to find relief with a team that actually cares? Contact Painless Medical Practice today to schedule your consultation!
Our Insurance Partners








FAQs About Headache Treatment
What Causes Headaches?
Headaches can have various causes, including stress, dehydration, muscle tension, sinus issues, and certain medical conditions. Migraine headaches have additional triggers such as hormonal changes, diet, and environmental factors. Understanding the cause of your headaches is important for effective treatment, and your healthcare provider can help identify potential triggers.
What Is the Best Treatment for Chronic Headaches?
The best treatment for chronic headaches often depends on the type and cause of the headache. Options may include medication, lifestyle changes, stress management, and therapeutic procedures like nerve blocks or Botox injections. A personalized treatment plan can be developed to address your specific symptoms and improve your quality of life.
How Effective Is Botox for Treating Migraines?
Botox has been shown to be effective in reducing the frequency and severity of chronic migraines. It works by blocking pain signals in targeted muscles, which helps to prevent migraine episodes before they start. Many patients experience noticeable improvement after a few sessions, with treatments usually spaced about 12 weeks apart.
Are There Any Side Effects to Nerve Block Injections for Headaches?
Nerve block injections for headaches are generally safe, but mild side effects can occur, such as temporary numbness, tenderness at the injection site, or minor discomfort. Serious side effects are rare, and most patients tolerate the procedure well. Your doctor will discuss any potential risks and guide you through the treatment process.
How Can I Prevent Recurring Headaches?
Preventing recurring headaches often involves a combination of lifestyle changes, such as managing stress, maintaining a regular sleep schedule, staying hydrated, and avoiding known triggers. Regular exercise and dietary adjustments can also help. Working with a healthcare provider can provide additional strategies and treatments tailored to reducing the frequency of your headaches.
What People Say About Us
our services before

If you are looking for a knowledgeable, compassionate and highly skilled professional, I highly recommend Dr Tymouch. His expertise truly stand out!
Dr. Tymouch took the time to carefully explain everything, answer my questions, and made me feel completely at ease throughout the entire visit. He treated my knee pain with injections, and the results were truly amazing and fast. I happy that I will be able to enjoy my vacation without discomfort. I’m so grateful for his care and highly recommend Dr. Tymouch to anyone in need of expert, compassionate treatment.
The team is professional, compassionate, and highly skilled at managing different types of pain.

